Background: Tisagenlecleucel (tisa-cel; autologous anti-CD19 CAR-T cell therapy) has demonstrated durable responses and a manageable safety profile in adult pts with r/r DLBCL in the JULIET trial. Here we report updated efficacy results with a 40 month median follow-up and associations with baseline Myc overexpression in tumor and tumor microenvironment (TME) characteristics.
Methods: JULIET is a global, phase 2 trial of tisa-cel in adult pts with r/r DLBCL. The relationship between Myc overexpression (Myc+: >40% by immunohistochemistry [IHC]), TME characteristics (including CD3+ T-cell infiltration, myeloid-derived suppressor cells [MDSCs], and LAG3 expression by fluorescent IHC) with efficacy outcomes (Month 3 [M3] response, duration of response [DOR], progression-free survival [PFS], and overall survival [OS]), and genomic mutation profile with M3 response were assessed.
Results: As of February 20, 2020 (median follow-up of 40.3 mo), 115 pts received tisa-cel infusion. Among the 61 pts with a response, the relapse-free probability was 60.4% at 24 and 30 mo; median DOR was not reached (95% CI, 10-not estimable [NE]). Median OS among all 115 infused pts was 11.1 months (95% CI, 6.6-23.9). Survival probability at 12, 24, and 36 months was 48.2%, 40.4%, and 36.2%, respectively. Median OS of pts with CR (n=37) or PR (n=7) at M3 was not reached; 80% of CR pts had an OS benefit of 20 months or longer. No new safety signals were detected. Of the 23 pts with ongoing CR and B-cell count available, 11 had CD19+ B cells recovered back to normal after 1 year, with similar patterns observed for CD20+ and CD22+ B cells.
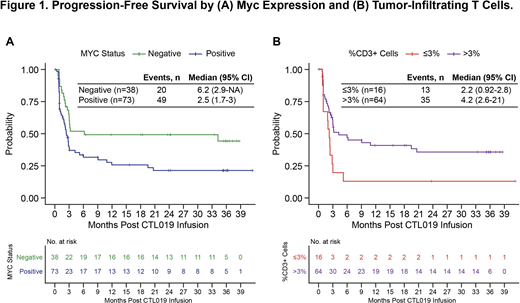
Of 111 pts whose baseline archival tumor biopsies were tested for baseline Myc expression, 73 were Myc+ and 38 were Myc−. Baseline Myc− status was associated with improved outcomes compared with Myc+ pts, including longer median DOR (not reached vs 19 months [95% CI, 3.4-NE]), PFS (6.2 months [95% CI, 2.9-NE] vs 2.5 months [95% CI, 1.7-3.0]; Fig.1A), and OS (21 months [95% CI, 10-NE] vs 7.8 months [95% CI, 4.6-18]). In the TME analysis of baseline biopsy, lack or low frequency of tumor-infiltrating CD3+ T cells (cutoff of ≤3%; n=16) was associated with shorter median PFS (2.2 months [95% CI, 0.92-2.8] vs 4.2 months [95% CI, 2.6-21]; Fig.1B) and OS (7 months [95% CI, 1.8-12] vs 21 months [95% CI, 6.7-NE]) compared with pts with >3% CD3+ T cells (n=64). Interrogation of checkpoint molecule expression on tumor-infiltrating CD3+ cells revealed that pts with the highest frequency of LAG3+CD3+ cells out of entire CD3+ T cell population (cutoff of >20%; n=12) at baseline had decreased median PFS (2.1 [95% CI, 0.82-3.1] vs 4.2 months [95% CI, 2.4-21]) and OS (4.3 [95% CI, 2.7-10] vs 21 months [95% CI, 10-NE]) compared with pts with ≤20% LAG3+CD3+ T cells (n=68). No differences in baseline clinical characteristics were observed in subgroups by Myc, CD3+, and LAG3+CD3+ expression. Additionally, in a small dataset, pts with the highest frequency of CD11b+HLA-DR− cells that represent MDSC phenotype at baseline were enriched with nonresponders.
In a survival tree analysis including infiltrating T cells, LAG3+ CD3+ cells, Myc, and LDH, pts with Myc− status and normal pre-infusion LDH levels (n=16) had longer PFS compared with normal LDH and Myc+, and pts with LDH 1- to 2-fold or >2-fold above the upper limit of normal, with the latter group having a poor PFS.
Whole exome sequencing of 46 baseline tumor samples was performed. No significant association with response was observed in mutations at the single-gene level. The correlation between molecular subtypes and M3 response was also investigated. Samples grouped into newly identified DLBCL subtypes (Chapuy et al. Nat Med. 2018; Schmitz et al. N Engl J Med. 2018; Wright et al. Cancer Cell. 2020) did not reveal an association with response, although the small sample size may limit interpretation.
Conclusions: Updated long-term data with 40 months median follow-up from the JULIET trial demonstrate sustained benefit in responding pts; in particular 80% of CR pts had a long-term OS (≥20 months). Taken together, the results suggest that Myc overexpression, or an unfavorable immunosuppressive TME with restricted T-cell response, may impact CAR-T cell efficacy in pts with DLBCL.
Jaeger:AbbVie: Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Gilead: Honoraria, Research Funding; BMS/Celgene: Consultancy, Honoraria, Research Funding; Karyopharm: Honoraria; CDR Life AG: Consultancy, Research Funding; Miltenyi: Consultancy, Honoraria; F. Hoffmann-La Roche: Honoraria, Research Funding. Bishop:Incyte: Honoraria, Speakers Bureau; CRSPPR Therapeutics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Autolus: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding; Kite: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; BMS: Honoraria, Speakers Bureau. Salles:Autolus: Consultancy, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria, Other: Educational events; BMS: Honoraria; Merck: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Educational events; Novartis, Servier, AbbVie, Karyopharm, Kite, MorphoSys: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Educational events; Roche, Janssen, Gilead, Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Educational events; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Educational events; Epizyme: Consultancy, Honoraria. Schuster:Novartis, Genentech, Inc./ F. Hoffmann-La Roche: Research Funding; AlloGene, AstraZeneca, BeiGene, Genentech, Inc./ F. Hoffmann-La Roche, Juno/Celgene, Loxo Oncology, Nordic Nanovector, Novartis, Tessa Therapeutics: Consultancy, Honoraria. Maziarz:Incyte, Kite, BMS/Celgene, PACT Pharma, Orca BioSystems, and Omeros: Honoraria; Novartis and Juno: Research Funding; Novartis and Athersys: Other: DSMB participant; Novartis, Incyte, CRISPR Therapeutics, Artiva Biotherapeutics, and AlloVir: Consultancy; Athersys: Patents & Royalties. Han:Novartis Pharmaceuticals Corporation: Current Employment. Savchenko:Novartis Pharmaceuticals Corporation: Current Employment. Roscoe:Navigate BioPharma Services, Inc., a Novartis Subsidiary: Current Employment. Orlando:Novartis Institutes for BioMedical Research: Current Employment. Knoblock:Novartis Pharmaceuticals Corporation: Current Employment. Tiwari:Novartis: Current Employment. Bubuteishvili Pacaud:Novartis: Current Employment. Corradini:Daiichi Sankyo: Consultancy, Honoraria; Celgene: Consultancy, Honoraria, Other: Travel and accommodations paid by for; Gilead: Consultancy, Honoraria, Other: Travel and accommodations paid by for; Incyte: Consultancy; Janssen: Consultancy, Honoraria; Kite: Consultancy, Honoraria; KiowaKirin: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Other: Travel and accommodations paid by for; F. Hoffman-La Roche Ltd: Consultancy, Honoraria; Sanofi: Consultancy, Honoraria; Servier: Consultancy, Honoraria; Takeda: Consultancy, Honoraria, Other; BMS: Other; AbbVie: Consultancy, Honoraria, Other: Travel and accommodations paid by for; Amgen: Consultancy, Honoraria, Other: Travel and accommodations paid by for.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal